By: Melanie Livet, Tashani Gaskins, and Chloe Richard
*This is a republished article. Names and titles have been updated as applicable.*
One of the most pressing challenges confronting the United States (US) healthcare system is delivering high-value, effective clinical interventions that improve health outcomes for patients. There has been a recent shift toward a value-based, also known as quality-based, healthcare approach that represents a tremendous opportunity to improve patient care through the creation of innovative care delivery models. To foster and advance these new models of care, it is key to explore ways to improve patient access to care and scalability of interventions. Community pharmacies can facilitate patient access to innovative evidence-based care, based on evidence supporting the ability of pharmacists to provide high quality patient care interventions1.
The UNC Eshelman School of Pharmacy Division of Practice Advancement and Clinical Education (PACE) has been working on a new project specifically focused on facilitating the uptake of quality-based services into community pharmacy. The purpose of this new project, funded by the National Association of Chain Drug Stores (NACDS) Foundation, is to improve patient care and population health. More specifically, the project team aims to:
identify, implement, and evaluate the feasibility and effectiveness of four patient-centered, quality-driven care clinical interventions delivered in community pharmacies.
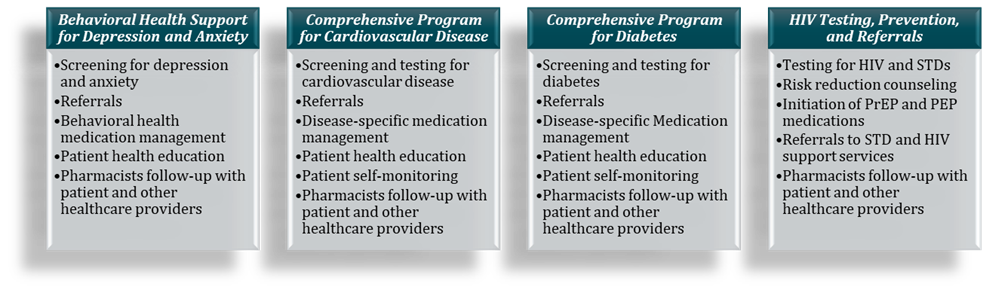
These four clinical interventions were carefully selected during the first few months of the project based on an evidence-based approach that identified current gaps in population health management2,3, coupled with interventions that are appropriate and potentially highly scalable in the community pharmacy setting4,5.
The Four Clinical Services Include:
Three of the four interventions (behavioral health support for depression and anxiety, comprehensive program for cardiovascular disease, and comprehensive program for diabetes) will be implemented within 2-3 pharmacy networks each, with two to five individual pharmacies per network. A diverse set of community pharmacies across the U.S. have been recruited. Pharmacies will deliver the services for twelve months. Toolkits are have been created to outline the services and facilitate implementation. Additionally, pharmacy staff will have access to a number of implementation support strategies, including trainings, ongoing coaching, implementation resources, and opportunities to share their successes throughout the project. To evaluate the feasibility and impact of these interventions, the team will examine both implementation and effectiveness outcomes, which may include medication adherence, relevant clinical metrics, patient and pharmacist satisfaction, and healthcare utilization.
The PACE project team is also working with a group of healthcare experts to foster long-term sustainability of these clinical interventions. This group is tasked with preparing the healthcare ecosystem to facilitate uptake and integration of quality-based innovations for patients in community pharmacies. This project has the potential to fill key gaps in current population health models by expanding delivery of evidence-based patient interventions at the local, community level.
Interested in learning more about this project?
Come back here to check out future blogs and follow us on twitter, @unc_pace, for future project updates. Read more about the project here.
Melanie Livet is the project principal investigator and implementation scientist/research assistant professor in PACE.
Tashani Gaskins is the former research and operations project director in PACE.
Chloe Richard is a research assistant with NIRN.
References:
- Goode J-V, Owen J, Page A, Gatewood S. Community-based pharmacy practice innovation and the role of the community-based pharmacist practitioner in the United States. Pharmacy. 2019;7(3):106. doi: 10.3390/pharmacy7030106
- Omboni S, Caserini M. Effectiveness of pharmacist’s intervention in the management of cardiovascular diseases. Open Heart. 2018 Jan 3;5(1):e000687. doi: 10.1136/openhrt-2017-000687.
- Thakur T, Galt KA, Siracuse MV, Fuji KT, Bramble JD. National survey of diabetes self-management program coordinators views about pharmacists’ roles in diabetes education. JAPhA. 2020;60(2):336-43.
- Gubbins PO, Klepser ME, Adams AJ, Jacobs DM, Percival KM, Tallman GB. Potential for pharmacy–public health collaborations using pharmacy-based point-of-care testing services for infectious diseases. Journal of Public Health Management and Practice. 2017;23(6): 593-600. doi: 10.1097/PHH.0000000000000482
- Shonesy BC, Williams D, Simmons D, Dorval E, Gitlow S, Gustin RM. Screening, brief intervention, and referral to treatment in a retail pharmacy setting: The pharmacist’s role in identifying and addressing risk of substance use disorder. J Addict Med. 2019;13(5):403-407. doi: 10.1097/ADM.0000000000000525